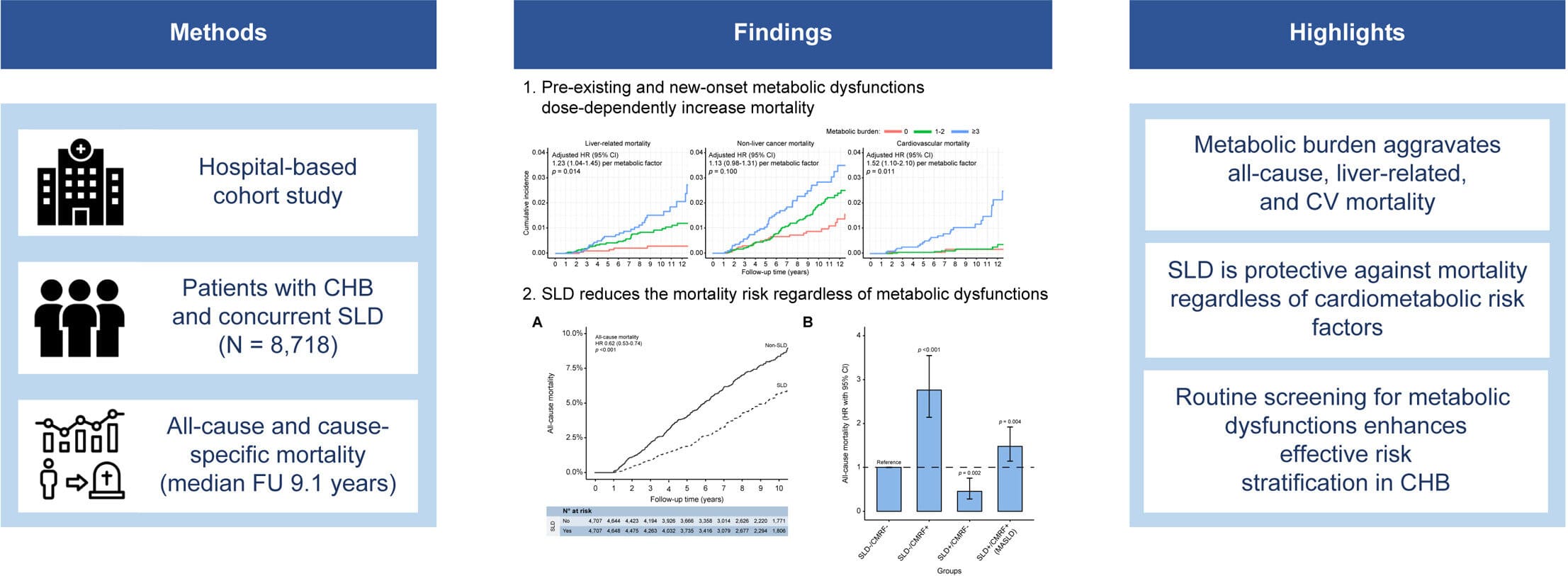
A study from National Taiwan University Hospital has unveiled how metabolic dysfunction significantly influences the mortality risks of patients with chronic hepatitis B (CHB). The research, recently published in the Journal of Hepatology, analyzed data from over 8,000 CHB patients over a 15-year period, highlighting the crucial role of metabolic health in liver disease outcomes.
The study found that CHB patients with concurrent steatotic liver disease (SLD) face a complex relationship between metabolic dysfunction and long-term survival. Those with metabolic disorders—such as diabetes, hypertension, and obesity—exhibited a markedly higher risk of all-cause, liver-related, and cardiovascular mortality. Notably, a higher cumulative metabolic burden was associated with a dose-dependent increase in mortality risks.
Among the metabolic disorders examined, diabetes mellitus was the most critical factor, with poorly controlled blood glucose levels (HbA1c > 8.0%) leading to a fourfold increase in liver-related mortality compared to those with well-controlled glucose levels (HbA1c < 6.0%). Additionally, patients who developed new-onset diabetes or hypertension during the follow-up period faced an even greater risk of death, emphasizing the importance of early diagnosis and proactive metabolic management.
"Patients with chronic hepatitis B who develop metabolic disorders are at significantly greater risk of death, especially those with multiple metabolic conditions," said Prof. Tung-Hung Su from National Taiwan University Hospital, the lead author of the study.
"Our findings emphasize the urgent need for routine metabolic screening and early intervention in this population. Metabolic health is not just an ancillary concern in chronic liver disease—it plays a direct role in determining long-term patient outcomes."
Unexpected protective effect of non-metabolic steatotic liver disease
Surprisingly, the study also revealed that CHB patients with SLD but without metabolic abnormalities had a lower risk of mortality compared to those without SLD. This suggests that hepatic steatosis, in the absence of metabolic dysfunction, might have a protective effect against long-term liver-related complications.
"This was an unexpected finding," said Dr. Shang-Chin Huang, from National Taiwan University and first author of the study. "While steatotic liver disease is generally considered a risk factor for liver-related complications, our results indicate that when it occurs without metabolic dysfunction, it might actually reduce mortality risks in CHB patients. This aligns with some of our previous research, which suggests that liver fat accumulation might, in some cases, be associated with improved clearance of hepatitis B virus."
Clinical implications and recommendations
Given the strong association between metabolic dysfunction and increased mortality, the researchers emphasize the importance of regular metabolic health monitoring for CHB patients. In particular, the study found that new-onset diabetes, hypertension, and excessive weight gain during follow-up further exacerbated mortality risks.
For patients with CHB, the study underscores the need for routine screening for metabolic dysfunction, including BMI, blood sugar, blood pressure, and lipid levels. Early intervention for those with metabolic disorders is needed to prevent long-term complications.
This study adds a new dimension to the understanding of metabolic dysfunction's role in chronic liver disease and calls for an integrated approach in managing hepatitis B patients. The results have drawn global attention in the hepatology field, providing critical insights for future research and public health strategies.
"Our findings have significant implications for the clinical management of hepatitis B patients," added Prof. Tung-Hung Su. "Beyond antiviral treatment, managing metabolic health should be a key component of hepatitis B care to improve patient outcomes."
More information: Shang-Chin Huang et al, All-cause and cause-specific mortality in patients with chronic hepatitis B and concurrent steatotic liver disease, Journal of Hepatology (2024). DOI: 10.1016/j.jhep.2024.12.009